- +353 1 797 9545
- Cian House, 1 Cian Park, Drumcondra, Dublin 9, D09 K7F8
There are numerous causes of shoulder pain. The following are some of the most common examples, and gives links should you wish to get some further information for your specific problem. Not all pain felt around the shoulder region is coming from the shoulder joint.
Referral of pain from the neck (cervical spine) is often accompanied by pain around the top of the shoulder blade . Pain in your shoulder that is caused by neck dysfunction could either refer as far as your shoulder, and/or into the shoulder and down the arm.
Pain may be either referred from the muscles and joints (somatic structures) or from nerve tissue. Pain coming from the shoulder itself, is often felt at the top of the arm. A common complaint is pain with lifting the arm or on pushing/pulling activities, which can be caused by the rotator cuff /bursa/tendonitis/tendonosis- this is known as rotator cuff related shoulder pain. Pain with sudden movements, at the end range of movements and increasing stiffness in the shoulder, may be signs of a frozen shoulder.
The junction between the end of the collar bone and the shoulder blade (A/C joint) can be injured with contact sports and trauma. Shoulder dislocations and fractures may also result from trauma.
Arthritis of the shoulder joint can occur due to degenerative changes (osteoarthritis) after the age of 60 or in those with a history of shoulder trauma. A less common type of arthritis, inflammatory arthritis (such as rheumatoid arthritis) can also manifest in the shoulder. Some shoulder pain may be referred from organs elsewhere in the body (visceral referral.)
For example, gallbladder pain or irritation of the diaphragm can manifest as pain into the tip of the shoulder. This list is just some of the most common examples, but in fact there are many more! This is where a comprehensive history and examination by a clinician with expert knowledge of the shoulder is so important.

Physiotherapy helps to restore normal, pain free movement. In order to do this effectively, it is really important that we take a comprehensive history and conduct a full examination to determine the exact problem (there are many different types of problems that cause shoulder pain.)
We can then design a specific treatment plan for you, often including a combination of manual therapy, exercise and advice regarding your environment/training. You do not necessarily need imaging (e.g X-ray or MRI) to start physiotherapy.
However we will advise you if we think imaging would be helpful. You can attend physiotherapy without referral from a Doctor.
Tendinopathy can be acute (recent occurance) or chronic (lasting for weeks or months). It is where there is degeneration or inflammation of the tendons, which causes pain.
This may be caused in some cases by repetitive overhead activities, a recent increase in shoulder exercise, or even a return to previous levels of activity, after a long period of inactivity.

This is where one of the rotator cuff muscles or tendons tear partially or fully. This can happen due to a trauma, degeneration, or indeed from repeated microtraumas.

You may hear the above terms in relation to shoulder pain. Sometimes in reports such as an MRI report, bursitis may be reported, or sub-acromial impingement.
A recently published International Consensus Paper (Requejo-Salinas, Lewis et al, 2022) recommended that the above three terms were not clinically useful and that the term “Rotator Cuff Related Shoulder Pain” be an overarching term to include ‘bursitis’ and ‘impingement’.

What is it?
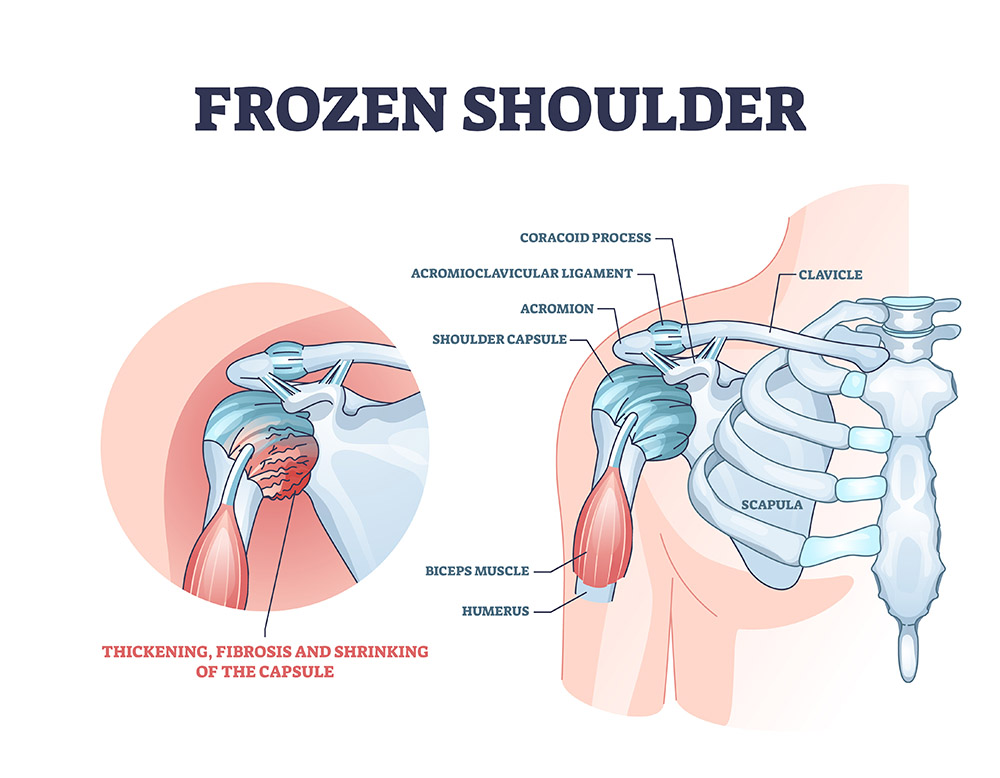
Also known as “adhesive capsulitis”, frozen shoulder is a condition that occurs when the connective tissue surrounding the shoulder joint (the capsule) becomes inflamed, thickened and eventually stiff.
Patients suffering from frozen shoulder will often notice pain at the top of the arm, (it can radiate down the arm if more severe), increasing loss of movement and stiffness. Typically, the symptoms come on gradually and worsen over time. Pain can often be worse at night and may disrupt sleep, which is often the part that patients find the hardest to cope with. Frozen shoulder is listed by the NHS as one of the top 20 most painful conditions that people may experience (Laguipo, 2019).
Symptoms from frozen shoulder typically progress through 3 overlapping stages of pain, stiffness and recovery and in some cases may last up to three years. This is an estimated time frame, and prognosis can vary depending on early diagnosis and access to optimal treatment.
How is frozen shoulder diagnosed?
Frozen shoulder is normally a clinical diagnosis. It is important to get a thorough clinical assessment if you have a painful and/or stiff shoulder, as other conditions may have similar signs and symptoms to a frozen shoulder in the early stages. It is quite common that patients present with pain at the top of the arm with certain movements, not realising that this pain is coming from their shoulder.
X-ray or MRI is useful to rule out other conditions such as arthritis (common after 60 yrs), avascular necrosis, dislocation etc. Actions like putting your arm into your jacket, reaching overhead, reaching to the side or trying to put your hand in your back pocket may become increasingly difficult or impossible. Sudden jerky movements can often illicit severe pain.
An early diagnosis of frozen shoulder is important, as accessing optimal treatments early can help alleviate symptoms.
Who gets frozen shoulder?
The most frequent age of onset of frozen shoulder is in the fifth decade (with women more commonly affected than men), however it can present between 30 and 70 years old. The exact cause of frozen shoulder is unknown. Some people develop a frozen shoulder for no identifiable reason (primary frozen shoulder.) Secondary frozen shoulder can also occur for a variety of reasons, for example: following trauma to the shoulder, injury to the rotator cuff, prolonged immobility of shoulder, after a stroke affecting the upper limb, diabetes etc. The likelihood of developing a frozen shoulder is significantly higher in those with diabetes.
How is it treated?
There are different treatment options available and it is important that you make a decision regarding your management plan that you are comfortable with following discussion with your physiotherapist. Some people choose to opt for physiotherapy alone (usually manual therapy and exercises.)
However, an intra-articular (IA) corticosteroid injection in addition to Physiotherapy in patients with frozen shoulder less than 1-year is associated with significantly better outcomes. A systematic review and meta-analysis on the management of frozen shoulder in 2020, found that IA corticosteroid injections were associated with improvement in pain and range of motion compared with no treatment or placebo. IA corticosteroid injections with physiotherapy were superior to IA corticosteroid injections alone (Challoumas et al, 2020). The publication examined 65 studies that included 4,097 patients. The timing of intervention is important. The injection is thought to reduce inflammation in the synovium (lining of the shoulder joint) and therefore reduce pain and resultant scarring and stiffness which is why having the injection earlier is thought to be most beneficial.
Less commonly, in severe cases, whereby the above approach has failed, surgical intervention may be considered.
What should I do?
If you have pain in your shoulder/ top of your arm, seek assessment from your Chartered Physiotherapist early. Your Chartered Physiotherapist will take a detailed history of your symptoms and conduct a thorough examination of your shoulder.
We know from the current available evidence that the most effective treatment in the early phase of frozen shoulder is an ultrasound guided corticosteroid injection in conjunction with physiotherapy. However, we will discuss your options and what is most advisable for you, to help you make an informed decision. Physiotherapy commonly involves manual therapy, as well as guided exercises focused on improving the range of motion and function in your shoulder.
Where is it?
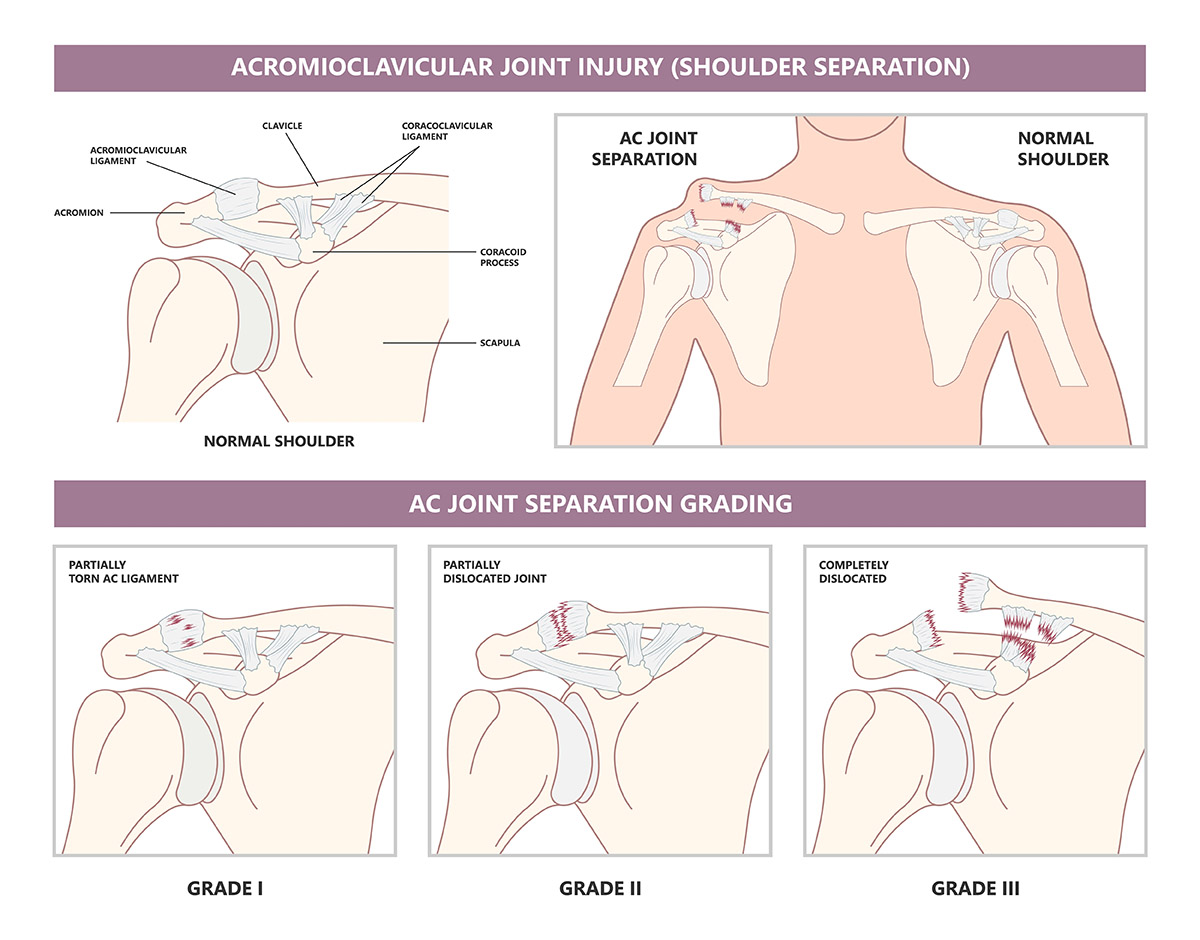
Also known as the AC joint, this joint is located where the collar bone (clavicle) and a part of the shoulder blade (called the acromion) meet. AC joint injuries represent roughly 10% of all shoulder injuries that seek medical attention. Traumatic injuries are common in collision sports such as rugby or due to an accident such as falling off a bicycle down onto the tip of the acromion.
Are there different grades of AC joint injury? How is it managed?
Severity of the injury is sometimes Graded from 1-6 (Rockwood Classification.) However, the Rockwood Classification has limitations including that it is based on radiological imaging only, that there is not complete consensus between Grade 3 and 5 injuries, and that it doesn’t take account of the level of pain, function or the demands that the person needs to be able to place on the shoulder. Surgical intervention is reserved for those with Grade 3 and upwards, with consideration being given to the demands that need to be placed on the shoulder. Cosmetic appearance is not an indication for surgery for most. All surgery carries risks, but this type of surgery is particularly challenging due to the proximity of important blood vessels and nerves.
Do I need physiotherapy?
Yes. For those that don’t have surgery, you will be placed in a sling initially (the time depends on the severity of the injury.) Taping and bracing of the AC joint can also be helpful for pain relief. Your physiotherapist will work with you to gradually restore movement and strength in your shoulder.
Even if you have a surgical stabilisation, you will still need physiotherapy after your operation. It is important that you are aware of this and commit to this prior to having your surgery. Your surgeon will have a specific protocol for you after your surgery, (depending on the degree of stabilisation surgery required) that will guide the length of time you will need to be in a sling after your operation and when you can start physiotherapy.
Who gets pain in the AC Joint?
In addition to injury following trauma, patients can also present with arthritis of the AC joint that causes pain. Depending on the type of arthritis, ultrasound guided injection may be helpful for pain relief in addition to physiotherapy.
I think I may have an AC joint injury, what should I do?
If you have had significant trauma and have obvious deformity of your shoulder (new big bump at the tip of your shoulder) then you should have imaging first (X-ray ray or MRI.) This is important to out rule an associated fracture and help determine if you will need surgery or not. The timing of your physiotherapy will depend on whether surgery is required or not. If your trauma was more
The first important thing to establish is what is wrong with your shoulder and what’s causing the pain. You may have had an MRI that reported a shoulder tendon tear/ tendonitis/tendonosis/rotator cuff tear or bursitis. For more information on this, click here Even if you do have rotator cuff related shoulder pain, the treatment is not a one size that fits all. There are different types of exercises for rotator cuff related shoulder pain, depending on your contributing factors, severity and the level of trauma involved. The more tailored your programme, the better the results.
Possibly. With any shoulder problem, people often notice a pain at the top of the arm (rather than in the shoulder blade at the back.) The predominant feature first with frozen shoulder is pain at the top of the arm at end range of shoulder movements. Pain usually starts before people notice that they’re losing shoulder movement. Once movement starts to reduce there is an equal loss of active movement (when you move your own shoulder) and passive movement (when we move your shoulder for you.) As the pain becomes more severe, it can radiate down the arm, often towards the base of the thumb. Other conditions also cause arm pain though, so on its own, arm pain is not a diagnostic feature.
This is the Acromioclavicular joint, where the end of the collar bone and a part of the shoulder blade meet. Pain here can be due to trauma or arthritis of this joint. Patients will often notice shoulder pain when lifting the arm overhead. For more information on AC joint injuries, click here
There are a few possibilities here, including that the pain has a “central source” and is referred out into both shoulders from your spine. Another potential cause is that you are doing something during your day that is simultaneously straining both shoulders (such as reaching too far forward to a keyboard with both arms.) Inflammatory arthritis is also a possibility, as the systemic inflammation affects both shoulders. This is where taking a detailed history and thorough examination is crucial for an accurate diagnosis, so that you get started on the best treatment for your shoulder pain.
Yes, however there are many different types of fractures that can be sustained around the shoulder. It is important that you bring your X-ray report or a note from your Orthopaedic Doctor detailing the type of fracture that you had along to your physiotherapy appointment. Shoulders are particularly prone to developing stiffness and poor movement if left immobile for too long, so it is important that you do not delay starting physiotherapy as soon as you are allowed. The term “fracture” is the medical term for a break or a “broken shoulder.” It is also very important that you move the joints below your shoulder while you’re waiting for it to heal (elbow, wrist, hand, fingers and thumb.) You must make a full fist and then straighten your fingers out fully several times per day and not just wiggle your fingers!!!!! Your physiotherapist can guide you with this type of exercises while you’re waiting to get started on your shoulder physiotherapy. That way, it will only be your shoulder that you will need to work on, instead of the whole upper limb becoming stiff, and you will end up needing less appointments.
Yes, at IONA Physiotherapy, all of the treating Physiotherapists hold a Masters in Physiotherapy and several years experience. We have also attended the Irish Shoulder and Elbow Society Conference over the years and hold membership of the Irish Shoulder and Elbow Rehabilitation Society. This helps us keep up to date with the latest developments, meaning that we can diagnose your problem accurately and come up with an effective treatment plan.
If your shoulder is uncomfortable/painful or not moving freely, make an appointment to come see us.
People generally need fewer physiotherapy appointments if they address a shoulder problem early.
We will want to see you move and examine your shoulder- so, it is best to wear loose fitting clothes that are easy to take on/off.
COSTS
€75 for initial appointments (includes assessment and treatment)
€75 for follow up appointments

IONA Physiotherapy Move With Ease Ltd. Trading as: IONA Physiotherapy.
Company registration no: 633072,
Cian House, 1 Cian Park, Drumcondra, D9,
Ciara Shields (Company Director)
Privacy Statement | © 2025 IONA Physiotherapy, Powered by Digital Media Center