Whether you love running, play team sports or enjoy staying generally active, calf muscle injuries are surprisingly common – and frustrating. If you’ve ever felt a sudden ‘pull’ or ‘tightness’ in the back of you lower leg, you may have experienced a calf strain (tear.)

Understanding your calf muscles
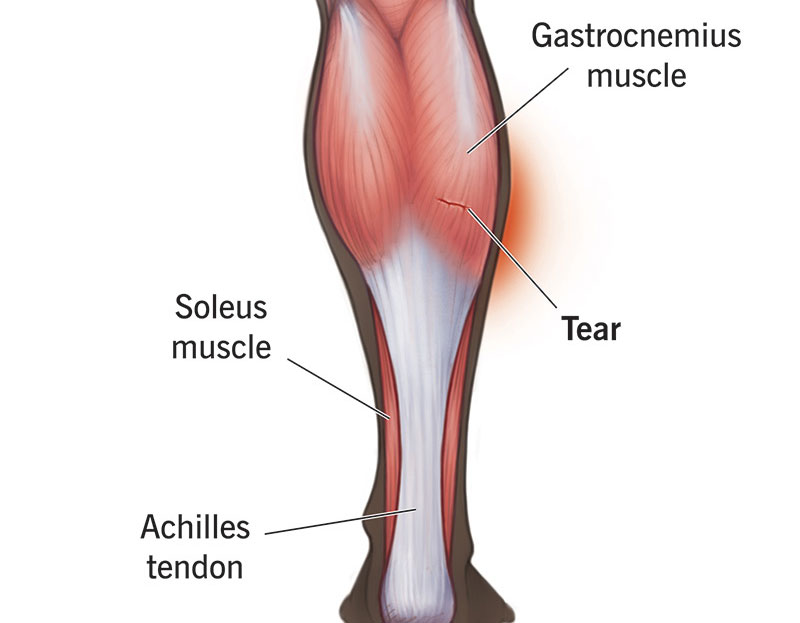
Your calf isn’t just one muscle – it’s a group of muscles working together. The two main calf muscles are:
- Gastrocnemius: This is the large, visible muscle at the back of your lower leg, and it is the most commonly injured.
- Soleus: A deeper muscle that supports the gastrocnemius. There are also smaller, deeper muscles that help control movement and stability.
These muscles are key for walking, running and jumping. When they are overloaded or not prepared for sudden movements, they can strain ( tear.)
Who gets calf injuries?
Calf strains happen to people of all ages at all levels of activities. They are most coming in the aged group of 40 to 60 years old, and more so for those in this category who play sports. This is often because:
- Muscles naturally lose some strength and flexibility with age
- The Achilles tendon can stiffen, putting extra stress on the calf muscles
- Training mistakes (like doing too much, too fast) are responsible for more than 60% of injuries in running.
How Calf injuries happen
Many people describe a sharp pain or a ‘pop’ in their calf while running, sprinting or jumping. Others notice a dull tightness that lingers after exercise. Sometimes, it feels like a bad cramp you can’t stretch out. If the pain doesn’t match a specific activity or moment, it may be worth checking other possible causes, like nerve or tendon issues.
Do you need a scan?
Good news – most calf strains don’t need medical imaging. A Chartered Physiotherapist can usually diagnose the injury through clinical assessment.
What recovery looks like
The key to a strong recovery isn’t just rest – its smart rehab. The best rehab will focus on:
Initial Deloading- you may need a graduated heel raise/ orthopaedic boot/crutches. A good gait pattern is crucial in the early days. No walking on your toes! Your physiotherapist will help you achieve this to speed up your recovery and prevent causing further injury.
Progressive loading: Start gently, then gradually increase the amount of stress on the muscle. Your physiotherapist will guide you through this step by step.
Consistency: Rehab starts at home but often progresses to gym-based exercises if your goal is to return to running or sport.
Milestones: Your calf should reach certain strength levels before moving to the next stage, like plyometrics (jumping drills) or running.
A Simple Strength test at home
A good way to measure calf strength (if not recently injured) is the single-leg heel raise – rising onto the ball of your foot slowly and lowering down.
- In your 20’s, men should aim for around 38 reps, women for 31
- In your 50’s, men should aim for about 24 reps, women for 23
- A difference of more than five reps between legs can signal weakness
Common rehab mistakes
People often get stuck because they:
- Walk around with a limp for days/weeks without seeking proper advice on how to achieve a good gait pattern while injured- straining the structures around the calf tear.
- Don’t add jumping / plyometrics back in towards the end of the program
- Don’t progressively increase loading (strengthening)
- Don’t assess their calf capacity (a Physio can do this) before returning to sport
Skipping these, increases your risk or re-injury, something we want to avoid.
The Bottom Line
Calf injuries are common but very treatable.
- Most involve the gastrocnemius muscle
- Scans are rarely needed
- A structured rehab plan with progressive loading is essential
Please make an appointment with one of our Chartered Physiotherapists on our online booking system here should you need an assessment.