.
Basketball is a non-contact sport, but this doesn’t make it a non-physical sport! As a sport, it involves complex movements including jumping, abrupt turns, changes of direction and deceleration, moderate- to full-speed running, side-stepping and back-peddling. Several research studies published looking at injuries in basketball have shown that the body parts that are most injured are the ankle and the knee (Andreoli et al., 2018; Clifton et al., 2018; Cumps et al., 2007; Zuckerman et al., 2018). The main focus for this blog will be ankle injuries, specifically lateral ankle sprains.

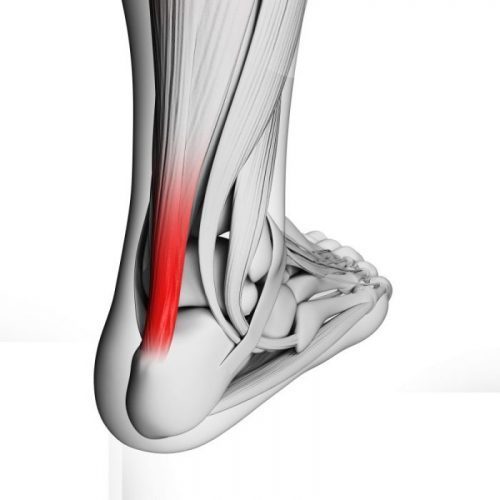
Lateral ankles sprains (LAS) occur on a sudden turning in of the ankle and foot (inversion) causing stress to the lateral structures of the ankle joint as bodyweight is put through it. This can happen if you jump in the air and land awkwardly, land on another player’s foot, or on sharp changes of direction. The most common ligament to injury in this way is the Anterior Talo-Fibular Ligament (ATFL) but other lateral ligaments and muscles groups, including the peroneal muscles tracking down the side of your shin and ankle, can be affected as well. ATFL attaches to the joint capsule of the ankle so swelling and bruising, is almost immediate for a lateral ankle sprain.
What should you do if this happens to you? As the rule goes, if in doubt, get it checked out! Ankle fractures happen in roughly 10-12% of lateral ankle sprains (Kerkhoffs et al., 2012). However, if there is bony tenderness at your ankle joint and/or at the smaller bones of the foot and you’re also not able to walk more than four steps, an X-ray is advisable. This is the recommendation from clinical guidelines called the Ottawa Ankle Rules regarding ankle X-rays following injury (see below).

On the other hand, if you’re able to put some weight through your ankle after you have “rolled” it but aren’t able to continue to train or play, it’s best to follow the POLICE principles (Bleakley et al, 2012):
P = Protection
In this instance, protection means sitting out of training or a game to “protect” your ankle from further injury. You may also require ankle taping carried, an ankle brace or support bandage, or even crutches. However, these, protection strategies should not be long-term.
O = Optimal L = Loading
Optimal Loading is not the same as rest. It is based on the evidence that “early activity encourages early recovery.” All this means is that you gradually start to move and weight-bear through your injured ankle as much as you can tolerate, early and often. If you only stick to “rest”, you run the risk of the ankle joint stiffening up, the muscles that help the ankle move may become deconditioned and your balance and ability to run/land/jump may be detrimentally affected, resulting in return to playing at a lower level than before you were injured. This in itself is a risk factor for further lateral ankle sprains.
I Ice
Ice helps your ankle sprain by promoting a pain-relieving, numbing effect to the injured area, and although somewhat controversial, is thought to reduce swelling. Avoid putting ice directly onto your skin – wrap it in a dampened towel or a dampened spare sock. If there is any numbness to your ankle post-injury or there is an open wound, do not apply ice.
C Compression
A simple tubigrip or elasticated support bandage may be useful at the acute and chronic stages of your ankle sprain to help with pain and possibly with swelling – it should be tight but comfortably so. Taping also comes under this category.
E Elevation
This is useful for swelling and pain management – and it’s a perfect time to do your rehabilitation exercises of gentle active ankle movements!
Usually minor to moderate ankle sprains take between 4 weeks and 2-6 months to fully recover. To prevent further ankle sprains, and to also prevent them occurring in the first place, balance and strength work for your ankles and lower limbs is crucial. This should include landing mechanics and multi-directional work. All of this rehabilitation is crucial so that the sensory nerve endings in your ankle and lower limb, feedback accurate and timely information to your central nervous system (including your brain), that the brain integrates this information well, so that the right message is sent to the correct muscles, at the correct time, and that your muscles are strong enough to act. This pretty impressive system is called sensorimotor control and is crucial to preventing re injury. Prophylactic taping and bracing of the ankle is also useful but should be used to complement your balance and strength work for the ankle, not replace it.
If you are returning to basketball, or any other sport, after an ankle sprain or need some advice regarding assessment and management of your current injury, contact us here at IONA Physiotherapy.
References
-
Andreoli, C.V., Chiaramonti, B.C., Buriel, E., Pochini, A.C., Einisman, V., Cohen, M. (2018) Epidemiology of sports injuries in basketball: integrative systematic review. BMJ Open Sport and Exercise Medicine, 27;4(1):e000468. doi: 10.1136/bmjsem-2018-000468. eCollection 2018.
- Bleakley, C.M., Glasgow, P., MacAuley, D. C., 2012. PRICE needs updating, should we call the POLICE? BJSM, 2012; 46(4): 220-221.
- Clifton, D.R., Hertel, J. et al. (2018) The First Decade of Web-Based Sports Injury Surveillance: Descriptive Epidemiology of Injuries in US High School Girls’ Basketball (2005-2006 Through 2013-2014) and National Collegiate Athletic Association Women’s Basketball (2004-2005 Through 2013-2014). Journal of Athletic Training, 53(11):1037-1048. doi: 10.4085/1062-6050-150-17.
- Cumps, E., Verhagen, E and Meeusen, R. (2007) Prospective Epidemiological Study of Basketball Injuries During One Competitive Season: Ankle Sprains and Overuse Knee Injuries. Journal of Sports Science Medicine, 6(2): 204-211. Published online 2007 June 1.
- Kerkhoffs, G.M. et al. (2012) Diagnosis, treatment and prevention of ankle sprains: an evidence-based clinical guideline. BJSM, 46:854–860. doi:10.1136/bjsports-2011-090490
- Taylor, J.B., Ford, K.R., Nguyen, A.D., Terry, L.M., Hegedus, E.J. (2015) Prevention of Lower Extremity Injuries in Basketball: A Systematic Review and Meta-Analysis. Sports Health, 7(5):392-8. doi: 10.1177/1941738115593441. Epub 2015 Jun 26.
- Zuckerman, S.L., Wegner, A.M., Roos, K.G., Djoko, A., Dompier, T.P., Kerr, Z.Y. (2018) Injuries sustained in National Collegiate Athletic Association men’s and women’s basketball, 2009/2010-2014/2015. BJSM, 52(4):261-268. doi: 10.1136/bjsports-2016-096005. Epub 2016 Jun 30.