Hamstring Muscle Injuries
If you are involved in sport, at any level, you will know someone who has had a hamstring injury, or you may have even had a hamstring injury in the past yourself.
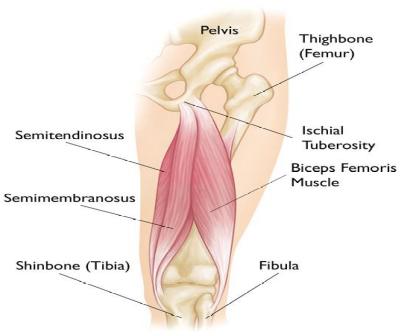
What are the hamstrings?
They are a group of muscles located at the back of your thigh. Their primary function is to flex (bend) the knee and extend (straighten) the hip. They also have other functions, such as stabilising the knee joint and the pelvis.
They are named Bicep Femoris, Semitendinosus, and Semimembranosus.
There is also a 4th muscle that blends with the hamstrings called Adductor Magnus

How do they get injured?
There are a few ways in which a hamstring can get injured, but typically the mechanism of injury may be:
-
Running / sprinting
-
Kicking
-
Bending over from the hip

Rehabilitation
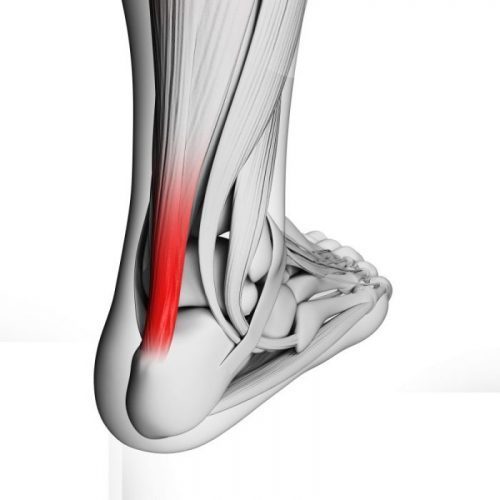
Adequate rehabilitation is essential, and your chartered physiotherapist will guide you through this process. The length of time from injury to a safe return to your chosen activity will largely depend on the severity of the muscle injury.
Muscle injuries are graded either: Grade I, Grade II, or Grade III.
Grade I muscle injury: A mild muscle strain
Grade II muscle injury: A partial muscle strain
Grade III muscle injury: A complete muscle tear or rupture
Thankfully the most common injuries are the Grade I and Grade II strains.
Rehabilitation Process
The overall aim of the rehabilitation period will be to strengthen your hamstring back to its pre-injury level and stronger.
Your physiotherapist will structure your rehabilitation into phases. Initially the goal will be to eliminate pain from walking and day to day activities. Once that landmark is achieved you can start loading (strengthening) your hamstring.
As the primary functions of the hamstring muscle group include flexing the knee and extending the hip, the strengthening exercises prescribed will reflect this.
Your program may include the following exercises:
-
Bridge
-
Squat
-
Split Squat
-
Deadlift
As well as strengthening exercises your physiotherapist will aim to include running as early as possible into your program. As you progress and get closer to full fitness some plyometric exercises will be added as well as some running drills.
Return to sport
You will set specific goals around return to sport with your physiotherapist. Your physiotherapist will explain and set out the specific criteria that you must meet in order to achieve these goals. This will help you understand your progress and achieve a successful outcome.