Knee osteoarthritis (OA) can be a challenging condition, impacting mobility and reducing the quality of life for many people.
Did you know that a chartered Physiotherapist can play an important role in managing knee OA?

Understanding Knee Osteoarthritis
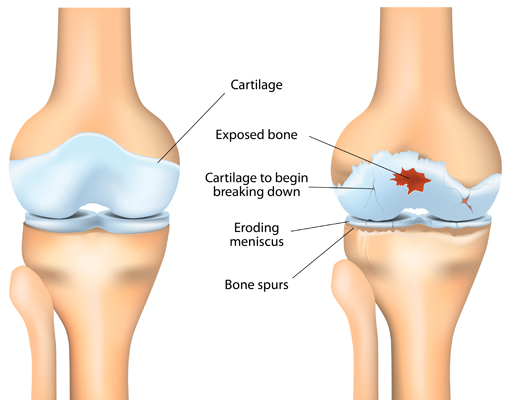
Before exploring the benefits of physiotherapy, it is important to have a basic understanding what osteoarthritis is.
OA is a degenerative disease that can affect the bone and cartilage in joints, making them stiff and painful.
There are many factors that can contribute to the development of OA, such as ageing, injuries, and even genetics.
The role of Physiotherapy
1: Pain management: Your Physiotherapist can employ various techniques to alleviate pain associated with knee OA. This may include manual therapy, such as joint mobilisations, to reduce stiffness and enhance flexibility.
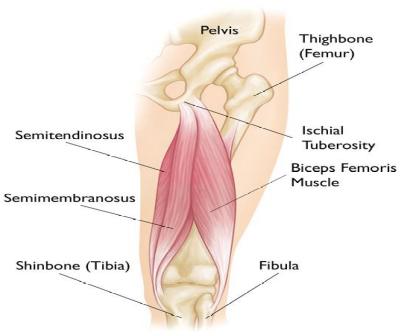
2: Exercise prescription: Specific exercise programs are a cornerstone of management for knee OA. Strengthening exercises to target the muscles groups that support the knee will help provide stability and support.
3: Education and self-management: Your physiotherapist will educate you on correct ergonomic advice, howe to protect the joint, and any lifestyle modifications that may be deemed appropriate. This can empower you to actively self-manage the condition.
4: Weight management: Excess weight can often put additional stress on joints, and as such, weight management strategies may form part of the overall holistic approach to managing OA.
5: Gait training: Abnormal gait patterns can exacerbate joint pain. Your physiotherapist can advise you should you need any assistance devices to limit any unnecessary exacerbations.
What's Next?
Physiotherapy is an important part of managing knee OA. Through a multi-faceted approach, encompassing pain management, exercise prescription, education, and lifestyle modifications, your Chartered Physiotherapist will empower you to take an active role in managing your condition.
If you have been diagnosed with osteoarthritis, please book an appointment with us by booking online here or calling us on 01 -797 9545